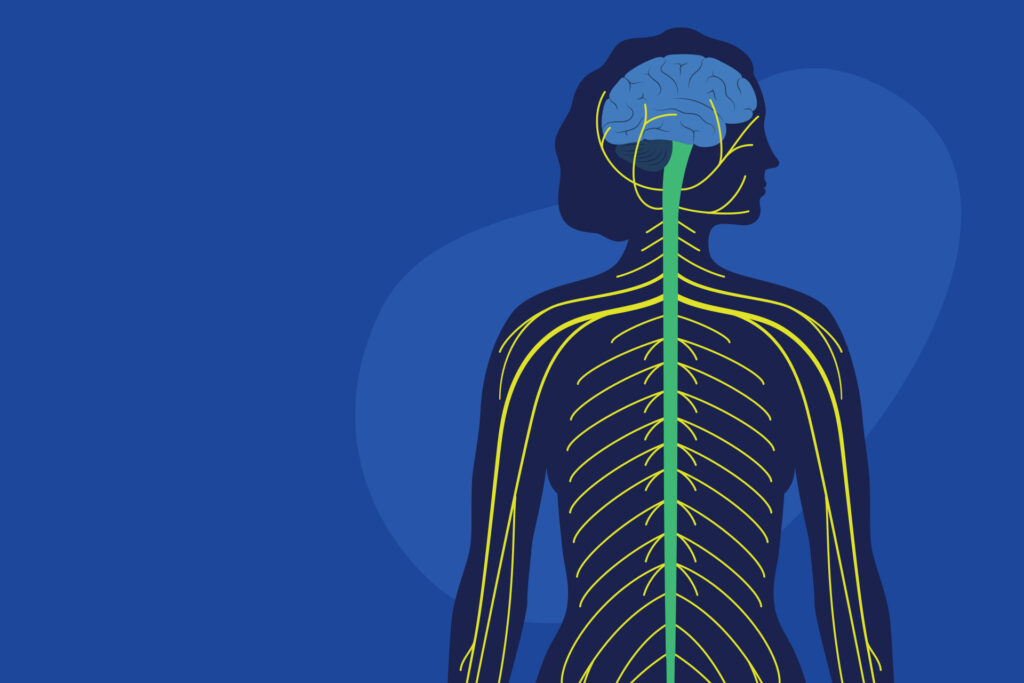
Amyotrophic lateral sclerosis (ALS), often referred to as Lou Gehrig’s Disease, is a rare, progressive, neurodegenerative disorder that affects nerve cells in the spinal cord and the brain. These motor neurons govern voluntary movement and muscle control. ALS causes motor neurons to degenerate and eventually die, resulting in muscle weakness, disability and eventually death. The average life expectancy of ALS patients is three to five years. It has an annual incidence of one to three newly diagnosed cases per 100,000 people in the U.S. The average age of diagnosis is 55-65 years old, although ALS can occur in people in their twenties. ALS was first identified in 1869 by French neurologist, Jean-Martin Charcot, but didn’t gain notoriety until New York Yankees legend, Lou Gehrig, was diagnosed with the disease in 1939. More recently, the “Ice Bucket Challenge”—a social media phenomenon where people would get doused with buckets of ice water—not only raised awareness for ALS but raised much needed funds which helped in the development of the latest drug used to treat ALS.
New Drug On the Block
On September 20, 2022, Amylyx Pharmaceuticals announced Relyvrio (sodium phenylbutyrate and taurursodiol) was approved to treat adults with ALS by the FDA. While this is the first new treatment in 5 years, it is not a cure. Relyvrio’s aim is to slow progression of the disease, potentially delaying death. Relyvrio is a fixed-dose combination of sodium phenylbutyrate and taurursodiol that work together to prevent nerve cells in the brain and spinal cord from dying prematurely. Relyvrio is supplied in single-dose packets for oral suspension that can be administered orally or via feeding tube. Initial dosing is one packet daily for the first 3 weeks, followed by a maintenance dose of one packet twice daily. Relyvrio can be taken by itself or added to other treatments.
A Bit of Controversy Swirling About…
As mentioned earlier, Relyvrio is not a cure for ALS, and there is still uncertainty on how efficacious this drug really is. Earlier this spring, the FDA’s Peripheral and Central Nervous System Drugs Advisory Committee (PCNSDAC) initially voted that data from the small Phase II Centaur trial did not show Relyvrio to be effective. However, the drug got an unusual second chance when the FDA extended its review period by 3 months to review additional survival analyses from Amylyx’s clinical trials. The PCNSDAC reconvened on September 2nd and voted to endorse Relyvrio based on the additional survival data. The FDA’s approval was based on the small Phase II CENTAUR trial and the CENTAUR open-label extension study which showed a 25% slowing of disease progression over a 24-week period. The additional survival data showed a median survival increase of 4.8 months. Amylyx has initiated PHOENIX, a Phase III trial that will evaluate the safety and efficacy of Relyvrio. This study is larger and longer in duration than the CENTAUR trial and should be completed in early 2024. Amylyx has committed to voluntarily pull Relyvrio from the market if the PHEONIX trial fails.
Although it is unusual for the FDA to approve a drug with such uncertainty around its efficacy, this level of uncertainty was deemed acceptable by the FDA advisory committee because of the seriousness and life-threatening nature of this disease and the substantial unmet need. While this decision may be understandable given the seriousness of this disease and the current unmet need, lowering the bar may have ramifications for other ALS drugs and beyond, especially if a fair amount of these drugs prove ineffective.
Besides the controversy surrounding its approval, there are questions around Relyvrio’s pricing and reimbursement. Amylyx Pharmaceuticals will price Relyvrio at $158,000 per year. This will put Relyvrio at a slightly lower price point than Radicava ORS, but still much higher than riluzole—two other drugs approved to treat ALS. The cost of Relyvrio is not surprising given the cost trend of new drugs used to treat rare conditions, but the high price tag—for a drug that may not even work—is hard to swallow. ICER (The Institute for Clinical and Economic Review), an independent nonprofit that analyzes the value of drugs, said that a cost-effective price for Relyvrio would be between $9,100 and $30,600 annually. Setting such a high price for a drug like Relyvrio with its questionable benefits may set a precedent for future ALS drugs with similar modest value.
Relyvrio is taken orally so most payers will reimburse under the pharmacy benefit. Amylyx said they will provide patient support services that will help commercially insured patients have minimal or no co-payments and no cost for uninsured or underinsured patients if they meet certain criteria. Amylyx is also working to facilitate comprehensive access through Medicare and Medicaid.
Not Many Options
There are very few drugs that are approved by the FDA to treat ALS, and they provide only modest benefits. There is currently no cure. The management of ALS is mainly supportive, which includes managing symptoms, nutritional support, and respiratory management. The following are the current pharmacologic treatments available today:
Riluzole
Riluzole was the first FDA-approved drug indicated to treat ALS. Originally approved in 1995 under the brand name Rilutek, manufactured by Clovis Pharma, the 50mg oral tablets are now available in generic form. Riluzole inhibits glutamate release and is the only FDA approved drug to have any impact on survival, prolonging life for approximately 3 months on average. The 2009 American Academy of Neurology (AAN) practice guideline stated that “riluzole was safe and effective for slowing ALS progression to a modest degree.” Riluzole is dosed at 50mg orally twice daily. It is well tolerated with the more significant adverse reactions being neutropenia and hepatic effects. The annual cost of generic riluzole is a very reasonable– $322 based on MAC pricing.
Tiglutik (riluzole) manufactured by ITF Pharma was approved in September 2018 by the FDA as the only thickened liquid formulation of riluzole. Approximately 80% of ALS patients have difficulty in swallowing because of muscle weakness in the face and throat. Riluzole was only available as oral tablets which had to be crushed for these patients. Available in a 50mg/10ml oral suspension, this liquid formulation offers the convenience of not having to crush pills, but at a cost of $38,240 (WAC) annually.
About a year later, Exservan (riluzole), an oral film formulation of riluzole was approved by the FDA in November 2019. Developed for ALS patients with swallowing difficulties, this oral film is placed on top of the patient’s tongue and dissolves without the need to swallow a pill or liquid. The annual cost of this product is $42,692 (WAC).
Edaravone
Radicava (edaravone), manufactured by Mitsubishi Tanabe, was approved by the FDA in 2017. It marked the first new treatment for ALS in 22 years since the approval of riluzole back in 1995. Edaravone is a free-radical scavenger that is thought to reduce oxidative stress, which plays a role in the development of ALS. The studies that led to its approval did not show an increase in overall survival but did show a slight decrease in the rate at which ALS worsened. Radicava is administered as an IV infusion of 60mg daily for 10 or 14 days every 28 days. The annual cost of Radicava IV maintenance dosing is $158,991 (WAC).
In May 2022, Radicava ORS, was approved by the U.S. Food and Drug Administration. This oral formulation of edaravone is a suspension which may be given either orally or via feeding tube following the same dosing schedule as the IV preparation. This oral option is much more convenient than the IV formulation with a cost of $165,351 per year for maintenance dosing. However, efficacy is similar to the IV formulation which is modest at best.
What’s on the horizon?
The Healey ALS Platform Trial is an innovative approach in ALS drug development. Instead of evaluating one drug at a time, the Healey Platform Trial is a multi-center, multi-regimen clinical trial that evaluates the safety and efficacy of several investigational drugs that are tested simultaneously and sequentially, in an ongoing platform trial design dictated by a single master protocol. This design maximizes resources and efficiency resulting in companies getting topline results more quickly at a lower cost. Ideally, this may translate into lower cost therapies. Zilucoplan, verdiperstat, CNM-Au8, pridopidine, and SLS-005 trehalose are currently in this trial. A couple of these drugs may be stopped because of negative data, but new drugs will be added as new investigational products become available.
Tofersen, by Biogen, is an antisense oligonucleotide that silences mutated genes for certain genetic forms of ALS. Biogen has announced the FDA has accepted the NDA and will render a decision on January 23, 2023. If approved, tofersen would be the first treatment to target ALS with genetic mutations.
Masitinib, by AB Science, is a selective oral tyrosine kinase inhibitor, which targets mast cells and microglia cells which are known to have a role in neuroinflammatory processes. A Phase II/III clinical trial showed masitinib, combined with riluzole, slowed decline by 27% compared to riluzole alone. Phase III confirmatory trials are ongoing. There is potential for approval in 2025.
There are several agents targeting various pathways to treat ALS in late phase development. We’ve only named a few. We’ll see if any of these drugs offer any improvements in slowing progression. The bigger question is whether any of these therapies can prolong survival.
In Conclusion
ALS is a terrible disease for which there is still no cure. We only have a small handful of drugs that have been approved to treat ALS. None of these drugs stop progression of ALS, they only modestly slow the rate of decline. Only riluzole, which happens to be the oldest treatment, is shown to have any impact on survival. The jury is still out on Relyvrio. While there is still some uncertainty about the drug’s efficacy, it does add another option to treat this disease where there is a vast unmet need. We await the results of the Phase III trial that is expected to conclude in 2024. Hopefully, Relyvrio proves to slow progression and extend life as the Phase II data suggests.
It remains to be seen if the approval of Relyvrio will set a precedent to allow other drugs for ALS, or other rare diseases, to be approved with questionable efficacy.