As the number of COVID-19 hospitalizations and deaths are trending downward and vaccines are currently showing efficacy in the U.S., it seems we are finally turning the corner. Some of the focus is shifting from the physical to the mental health impact of the pandemic. From the beginning of the COVID-19 pandemic, there was concern those affected by the virus may be at an increased risk for mental health issues. There was also early evidence showing COVID-19’s effect on the nervous system. Experts are now trying to prepare for the long-term impact of the neurological and long-term mental health implications caused by the pandemic.
Covid-19 Mental Health Impact by the Numbers
In 2019, just prior to the pandemic, 1 in 10 adults in the U.S. reported anxiety or depressive disorder. During this pandemic, the number has changed to 4 in 10 adults reporting symptoms of anxiety or depressive disorder. We’re seeing a magnification of mental health issues, caused both directly and indirectly by the pandemic.
Observational studies1,2 from a group of scientists at the University of Oxford showed that COVID-19 survivors had a greater risk of developing mood and anxiety disorders within 3 months of being diagnosed with COVID-19, and estimates that the overall incidence of neurological or mental health diagnoses is at 34% within 6 months of being diagnosed. The study found that the most common diagnoses were anxiety, mood and substance use disorders as well as insomnia. The incidence of neurological disorders was lower with ischemic stroke, dementia and brain hemorrhage leading the way. Disease severity also directly impacted risk. Those who experienced severe COVID-19 symptoms had a greater risk for mental health and neurological diagnoses. While the incidence of neurological disorders was much lower than mental health issues, this risk increased with the severe COVID-19 cases.
Mental health issues also impacted those that were not infected with the virus, but suffered mental health effects from the environment created by the pandemic. The COVID-19 pandemic combined with the ensuing social and financial burdens have negatively affected mental health and created new issues for people already suffering from mental health and substance use disorders. Several factors may be driving these increases. The continuous stress of unemployment, loss of housing, income, and food security, have threatened basic survival. Throughout the pandemic, people find themselves living with a constant sense of uncertainty which is associated with outcomes ranging from negative psychological well-being to elevated blood pressure. In addition, living with uncertainty magnifies the psychological impact of other stressors. A CDC report3 showed that 31% of respondents reported symptoms of anxiety or depression, 13% reported having started or increased substance use, 26% reported stress-related symptoms, and 11% reported having serious thoughts of suicide in the past 30 days. These numbers are almost double the rates we would usually see pre-pandemic. Although these are general numbers, we are seeing that different populations are at increased risk to develop or exacerbate mental health issues.
Emerging data is showing that the pandemic has not affected everyone equally. The pandemic has disproportionately affected minority communities. Studies show black and Hispanic adults are more likely to report symptoms of anxiety and/or depression compared to white adults. This is in addition to the higher rates of COVID-19 infections and deaths faced by these minority communities. This shows a need to continue working to address these long-standing disparities so that access to life-saving medical and psychiatric care is available to everyone.
Additionally, essential workers such as health care providers, grocers, and restaurant workers, have shown high rates of mental health issues. These workers do not have the luxury of working from home and are at risk of contracting the virus or exposing other family members. This coupled with the stress of financial uncertainties contribute to poor mental health outcomes for these workers. Essential workers are more likely than nonessential workers to report symptoms of anxiety or depressive disorder (42% vs. 30%, respectively), starting or increasing substance use (25% vs. 11%), or considering suicide in the past 30 days (22% vs. 8%)4.
Children Impacted by Covid-19 Mental Health Strain Too
Often forgotten in this mental health crisis caused by the pandemic are children. They too, are impacted by the stress their parents are feeling, and the disruption to their daily lives including school closures, suspension of sports and other social activities. And availability of and access to important mental health care and resources for children—often offered directly through the school system—has also been negatively impacted by school closures.
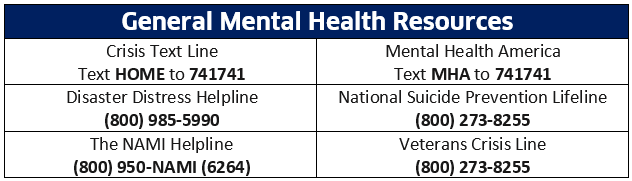
Even as new COVID-19 cases and deaths decline, the mental health impacts of COVID-19 may be long lasting, and are sure to leave a wave of shocks well beyond the pandemic itself. The need for increased mental health and substance use services will be needed long-term. It is important that the public be made aware of available help and resources and seek assistance at the appropriate time. Healthcare decision makers need to work together to apply evidence-based strategies to support the mental health needs of everyone and ensure these strategies are easily accessible, especially to those groups that are most vulnerable.
References
- Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2021;8(2):130-140.
- Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. The Lancet Psychiatry. 2021;8(5):416-427.
- Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049–1057. DOI: http://dx.doi.org/10.15585/mmwr.mm6932a1external icon
- 2021. The Implications of COVID-19 for Mental Health and Substance Use. [online] Available at: <https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/> [Accessed 14 May 2021].
.